Introduction

Acid reflux, also known as gastroesophageal reflux disease (GERD), is a chronic condition where stomach acid frequently flows back into the tube connecting your mouth and stomach (oesophagus). This backwash (acid reflux) can irritate the lining of your oesophagus. Many people experience acid reflux from time to time, and it’s generally manageable through lifestyle changes and over-the-counter medications. However, for some, it is a persistent issue that requires medical attention. This article explores the various aspects of acid reflux, including its causes, symptoms, risk factors, diagnosis, treatment, and prevention strategies.
Causes of Acid Reflux
Acid reflux occurs when the lower oesophageal sphincter (LES) – a ring of muscle at the bottom of your oesophagus – doesn’t function properly. Normally, the LES relaxes to allow food into the stomach and then tightens to prevent backflow. When the LES is weak or relaxes inappropriately, stomach acid can flow back up into the oesophagus, causing symptoms.
Common causes include:
- Dietary Factors: Consuming large meals or lying down right after a meal, eating a heavy meal and then lying on your back or bending over at the waist, eating certain foods like citrus, tomato, chocolate, mint, garlic, onions, or spicy or fatty foods, drinking certain beverages, such as alcohol, carbonated drinks, coffee, or tea.
- Lifestyle Factors: Smoking, being overweight or obese, eating close to bedtime, and stress.
- Medical Conditions: Pregnancy, hiatal hernia, and connective tissue disorders like scleroderma.
Symptoms of Acid Reflux

Acid reflux symptoms can vary, but common ones include:
- Heartburn: A burning sensation in the chest, usually after eating, which might be worse at night.
- Regurgitation: A sour or bitter-tasting acid backing up into the throat or mouth.
- Dysphagia: Difficulty swallowing.
- Chest Pain: Especially after bending over, lying down, or eating.
- Chronic Cough: Especially at night or after a meal.
- Laryngitis: Hoarseness or sore throat.
- Asthma Symptoms: Worsening asthma or new asthma in adults.
Risk Factors
Several factors can increase the risk of developing acid reflux:
- Obesity: Excess weight increases abdominal pressure, pushing stomach contents into the oesophagus.
- Pregnancy: Hormonal changes and pressure on the stomach from the growing uterus can cause acid reflux.
- Smoking: Smoking relaxes the LES and stimulates acid production.
- Medications: Certain medications, including aspirin, ibuprofen, muscle relaxers, and some blood pressure medications, can increase acid reflux risk.
- Dietary Habits: Consuming trigger foods and drinks, such as fatty or spicy foods, alcohol, and caffeine.
Diagnosis
To diagnose acid reflux, doctors may use several methods:
- Upper Endoscopy: A flexible tube with a camera is inserted down the throat to examine the oesophagus and stomach.
- Ambulatory Acid (pH) Probe Test: A monitor is placed in the oesophagus to identify when and for how long acid regurgitation occurs.
- Esophageal Manometry: Measures the rhythmic muscle contractions in the oesophagus when swallowing.
- Barium Swallow: X-rays of the upper digestive system after swallowing a barium solution.
Treatment Options
Treating acid reflux typically involves a combination of lifestyle changes and medications. In severe cases, surgery might be required.
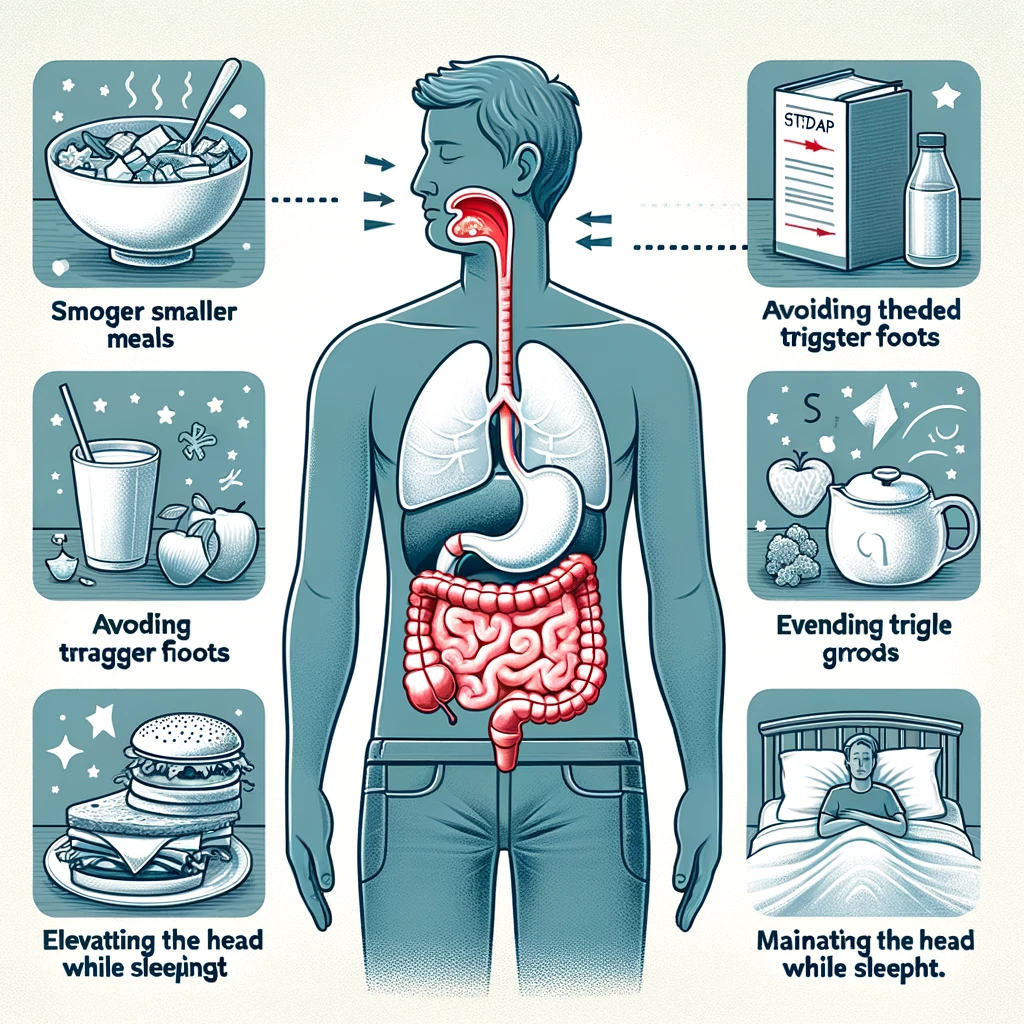
Lifestyle Modifications:
- Dietary Changes: Avoid trigger foods and beverages, eat smaller meals, and avoid eating before bedtime.
- Weight Management: Lose excess weight to reduce abdominal pressure.
- Quit Smoking: Smoking cessation can improve symptoms.
- Elevate the Head of Your Bed: Raising the head of your bed by 6 to 8 inches can prevent acid from flowing back into the oesophagus while sleeping.
Medications:
- Antacids: Neutralise stomach acid and provide quick relief. Examples include Tums, Rolaids, and Mylanta.
- H2 Receptor Blockers: Reduce acid production. Examples include ranitidine (Zantac) and famotidine (Pepcid).
- Proton Pump Inhibitors (PPIs): Block acid production and allow time for damaged oesophageal tissue to heal. Examples include omeprazole (Prilosec) and esomeprazole (Nexium).
- Prokinetics: Help the stomach empty faster. Examples include metoclopramide (Reglan).
Surgical Options:
- Nissen Fundoplication: The surgeon wraps the top of the stomach around the LES to tighten the muscle and prevent reflux.
- LINX Device: A ring of magnetic beads is wrapped around the junction of the stomach and oesophagus. The magnetic attraction between the beads keeps the junction closed to refluxing acid but allows food to pass through.
Complications of Acid Reflux
If left untreated, chronic acid reflux can lead to serious complications, including:
- Esophagitis: Inflammation that can damage tissues of the oesophagus.
- Esophageal Stricture: Narrowing of the oesophagus caused by damage from acid, leading to difficulty swallowing.
- Barrett’s Esophagus: A condition where the tissue lining the oesophagus changes to resemble the lining of the intestine, increasing the risk of oesophageal cancer.
- Esophageal Cancer: Particularly adenocarcinoma, a type of cancer associated with chronic GERD.
Prevention Strategies
To prevent acid reflux, consider the following strategies:
- Eat Smaller, More Frequent Meals: Avoid overloading your stomach.
- Avoid Trigger Foods and Drinks: Identify and steer clear of foods and beverages that trigger your symptoms.
- Stay Upright After Eating: Wait at least three hours before lying down or going to bed.
- Maintain a Healthy Weight: Reduce excess weight to decrease abdominal pressure.
- Quit Smoking: Smoking cessation can improve LES function and reduce acid production.
- Avoid Tight Clothing: Wear loose-fitting clothes to avoid pressure on your abdomen.
- Manage Stress: Engage in relaxation techniques such as yoga, meditation, or deep breathing exercises.
Living with Acid Reflux
Living with acid reflux can be challenging, but it’s possible to manage the condition effectively through a combination of lifestyle changes, medications, and regular medical check-ups. Here are some tips for managing acid reflux day-to-day:
- Keep a Food Diary: Track what you eat and drink, and note any symptoms that arise. This can help you identify and avoid trigger foods.
- Chew Gum: Chewing gum increases saliva production, which can help neutralise stomach acid.
- Stay Hydrated: Drink plenty of water throughout the day to help dilute stomach acid.
- Eat Slowly: Take your time to chew your food thoroughly and avoid rushing through meals.
- Elevate Your Head While Sleeping: Use a wedge pillow or elevate the head of your bed to reduce nighttime symptoms.
- Consult Your Doctor Regularly: Regular check-ups with your doctor can help monitor your condition and adjust your treatment plan as needed.
Conclusion
Acid reflux is a common but manageable condition. Understanding the causes, symptoms, and risk factors can help you take the necessary steps to prevent and treat this condition. By making lifestyle changes, taking medications as prescribed, and seeking medical advice when needed, you can reduce your symptoms and improve your quality of life. If you experience persistent or severe symptoms, consult a healthcare professional for a proper diagnosis and treatment plan.